What causes diverticular disease?
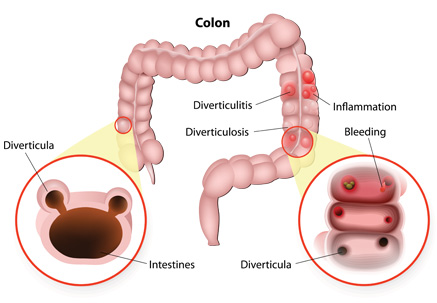
Diverticulosis or pocket formation in the colon is caused by high pressure within the colon. The high pressure in the colon is caused by straining during bowel movements which is most common with people that have a low fiber diet. The high pressure pushes on areas of the bowel wall that are weak causing pockets to form. It is these pockets that can then potentially rupture and lead to diverticulitis.
How is diverticular disease diagnosed?
Diverticulosis often causes no symptoms. To diagnose it, it is often seen during colonoscopy done by your doctor when it is indicated. To diagnose diverticulitis, you would need to be examined by a physician and may require additional tests including CT scan of the abdomen and pelvis to confirm the diagnosis and ensure there are no complications of it.
How is diverticular disease treated?
Most people live their whole lives with diverticulosis and do not have any problems. To prevent formation of these pockets in the first place, it is recommended to eat a diet high in fiber including fruits and vegetables, and to limit red meat.
If a patient presents with diverticulitis, the treatment is started with antibiotics either in pills or intravenously. Sometimes this may require admission to hospital and treatment with bowel rest and intravenous fluid hydration until the attack subsides.
- Diverticulitis with abscess can be treated with radiological drainage.
- Recurrent attacks of diverticulitis with constant antibiotic treatment requires surgery.
- Persistent abscess with peritonitis requires surgery.
- Fistula formation requires surgery.
- Stricture formation and obstruction requires surgery.
Surgery is performed using traditional open surgery or laparoscopic and robotic minimally invasive techniques. At the time of evaluation, your colorectal specialist will select the best option for you.