What are the symptoms of anal fissures?
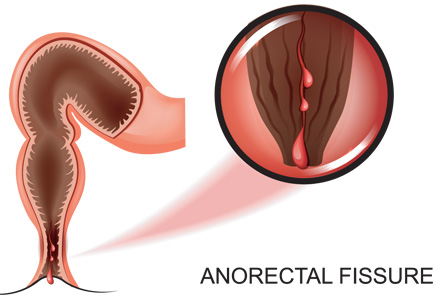
Classical symptoms are pain on or after defecation that may last from a few minutes to several hours. Often there is bright red blood on the toilet paper and patients may also complain of itchiness. The fissure may be seen on examination. Acute fissures are superficial splits in the anoderm. The distinction between acute and chronic fissures is arbitrary but the accepted definition is that fissures failing to heal within six weeks despite dietary measures are diagnosed as chronic. Chronic fissures have integrated edges and fibers of the internal anal sphincter may be visible at the base. A skin tag or Sentinel polyp may be present distally.
What causes anal fissures?
Although historically an anal fissure was thought to be caused by the passage of a hard stool bolus, this does not explain why the majority occur in the posterior midline. More recently, anal canal ischemia and anal hypertonia have been put forward as significant factors in the pathogenesis of chronic anal fissure.
How are anal fissures treated?
Acute fissures
Over 90% of fissures are acute and short-lived, resolving spontaneously or by treatment with dietary manipulation. Conservative methods of treating acute anal fissures include stool softeners, hot baths and topical anesthetic solutions with healing in over 85% of patients.
Chronic fissures
The majority of patients with long-standing chronic fissures requires intervention. Treatment has been targeted at reducing sphincter spasm and traditionally this has involved surgical intervention. Lateral sphincterotomy is a procedure where the internal sphincter is partially divided to decrease sphincter spasm. An alternative is chemical sphincterotomy which is achieved using Botox solution. Many fissures that do not heal with creams and where there is no spasm will respond to a simple surgical procedure to stitch close the fissure, called a fissurectomy. Our physicians can exam and discuss what would be appropriate for you.
Pharmacological treatment
Topical glyceryl trinitrate ointment, nifedipine and diltiazem creams have been used traditionally to help decrease anal spasm and encourage healing. Botulinum toxin A injected into the internal anal sphincter is also used to induce relaxation of the anal sphincter and encourage healing.
Surgical treatment
Many fissures simply become non-healing chronic wounds at risk for infection or fistula, and a simple excision and closure (fissurectomy) is appropriate. At times where there is scar and spasm a lateral sphincterotomy which involves division of the lower fibers of the internal anal sphincter is appropriate. An alternative surgical approach is the use of anal advancement flap which is applied particularly for chronic anal fissures that are not related to increased anal spasm. Your doctor will assess you and advise if this is an option for you.